Diagnosis
The diagnostic process with my brain tumour was probably a
year- long slog of confusion from start to finish. its not over yet either (no histology yet). It’s a bit of a long read so
you more than welcome to skip to the end because the end result is the same,
but for my own benefit I’m going to document the years process..
In summer of 2012 I started having panic attacks out of the blue while on medical leave from university due to a particularly bad spell of IBS that prevented me from attending enough lectures to be allowed to continue. Mostly due to this being an NHS funded course in which 20 weeks of work for the NHS was required per year as a diagnostic radiographer. So any time off sick was taken seriously. I’ve had IBS since I was 16 after a stomach infection picked up on a holiday in Portugal. It can be an extremely debilitating at times and often prevented me from doing normal stuff a teenager would want to do, but it wasn’t too bad.
The initial bout of severe anxiety lasted a few months and was brought under control with the use of beta blockers and cognitive behavioural therapy which was fantastic. I had my anxiety under a certain level of control ready to return to university by December 2012 with a moderate level of health anxiety that mostly related to physical symptoms that I would get frequently. It was an extremely odd time for me as I’ve always been a very confident person and mentally well. Having a mental health condition is a whole different ball game for me that took a lot of adjusting too. I refused all anti-depression anti-anxiety meds as I was fearful of the effect they would have on my life and I wanted to do it on my own.
In summer of 2012 I started having panic attacks out of the blue while on medical leave from university due to a particularly bad spell of IBS that prevented me from attending enough lectures to be allowed to continue. Mostly due to this being an NHS funded course in which 20 weeks of work for the NHS was required per year as a diagnostic radiographer. So any time off sick was taken seriously. I’ve had IBS since I was 16 after a stomach infection picked up on a holiday in Portugal. It can be an extremely debilitating at times and often prevented me from doing normal stuff a teenager would want to do, but it wasn’t too bad.
The initial bout of severe anxiety lasted a few months and was brought under control with the use of beta blockers and cognitive behavioural therapy which was fantastic. I had my anxiety under a certain level of control ready to return to university by December 2012 with a moderate level of health anxiety that mostly related to physical symptoms that I would get frequently. It was an extremely odd time for me as I’ve always been a very confident person and mentally well. Having a mental health condition is a whole different ball game for me that took a lot of adjusting too. I refused all anti-depression anti-anxiety meds as I was fearful of the effect they would have on my life and I wanted to do it on my own.
I rejoined university with under control anxiety but had
many physical symptoms (listed below) all of which were intermittently
presenting and were from time to time discussed with gp’s but for the most part
I would tell myself it’s just anxiety and continue to go about normal daily
activities.
Symptoms
Symptoms that occurred that year on a regular basis including: headaches, light-headedness, shortness of breath, anxiety, loss of balance, palpitations and varying heart rates, chest pain, and nightmares most nights. All symptoms intermittent throughout the year but always something going on that needed coping with every day really. Occasional bouts of depression, forgetfulness and missing words such as going to a pharmacist and picking up my prescription and being unable to recount my date of birth or just generally not having words come to my speech like i'd expect. All the symptoms can be caused by anxiety and i was more than happy accepting that this was just my problem. I often felt like I had a brain tumour or a heart arythmia throughout the year but thats what health anxiety is.
I didn’t go to the doctors as much as perhaps I should as I didn’t
want to come across as an even bigger hypochondriac. Also getting gp’s
appointments in Cardiff as a student travelling around all the time on
placement is extremely difficult in such an oversubscribed area of the country.
February 2013
Had further CBT during a bad patch for physical symptoms in which a counsellor suggested my symptoms which where chest pain and dizziness at the time sounded like a physical problem and not a health anxiety issue. This included a trip to the supermarket which made me so dizzy I needed help home. GP surgery appointments were over two weeks away so I went to out of hours gp in Cardiff based at the uhw a&e site. Was given chest x-ray and ecg, nothing to report back other than bradycardia and low blood pressure due to the propranolol.March 2013
Lowered
propranolol dose to 60mg to help with bradycardia. Started waking up
tachycardic frequently but would normally calm down an hour after first dose of
propranolol. Would be very disconcerting considering my resting heart rate is
normally in the 50’s to wake up with it in the 100’s. became a very regular
occurance which would effect my work in the mornings/ ability to get out of bed
and do day to day activities. Some days the fast heart rate would remain all
day long in the plus 100 zone. High heart rate put down to anxiety.
April 2013
Started feeling uneasy about going places/ walking due to
bouts of dizziness and lightheadedness. Travelling to placement going shopping
or town became issues that would cause anxiety for me. Started leaning on
trolleys to get round supermarkets. Stopped doing any heavy weightlifting as I
felt unsafe along with most cardiovascular exercise that would just make my head spin. Became a little depressed
with the situation and put on a lot of comfort weight. But was accepting that
it was all anxiety.
August 2013 beginning to realise -
September 18/2013
A seizure occurred walking back from a relatively
symptomless free day at work in Magnetic Resonance Imaging that day. Reached
the top of a flight of stairs and found myself on the floor having a seizure,
still fully conscious all the way through but again had no control of my left
side of my body. Took 10 minutes to recover the strength to get up and decided
to walk into A&E in which I was put on a waiting list for an mri and had a
cyst drained that was growing on the back of my head.extremely painful experience having a cyst drained, but it wasnt a pretty sight and needed to go. So I had a nice headwound bandage to go with my
time in hospital. Ecg taken, bloods taken,
high white blood cell count and a fever, discharged with a waiting list
for an MRI.
September 19/2013 the big day!
Had further seizures during the night upon waking from
nightmares, shook uncontrollably all night until 10am when I got up and shakily
got dressed and stumbled my way into work. Fortunately it’s a 5 minute walk,
but it took me a good 15 minutes of extremely shaky walking to get in to the
department. My walking hasn’t particularly improved since. Was due to return to A&E for
the cyst to be re-drained anyway. I Was given a CT head after telling A&E
about further seizures.
It was an extremely surreal experience being scanned in the
department I had worked in for 20 weeks by people who I knew. I wasn’t worried
at all jumping on the CT scanner, I’ve seen too many normal head scans for
people with my symptoms. All the staff were relaxed, I was relaxed. Nothing to
worry about, right?
I knew something was up after I’d been sitting on the
scanner for far too long after the scan had finished. The radiographers came in
to tell me that a radiologist was looking over my scans which I knew meant
there was something abnormal on my CT. They told me I would get an
immediate MRI with gadolinium contrast. This was the pit of the day. My brain
went straight into a black hole of shock. I knew there were still nice options.
It could be small. It could be a cyst or a hematoma. I knew I hadn’t had a
stroke. Waiting for the MRI was the most nerve wrecking half hour of my life.
The nurse who had accompanied me up from A&E was extremely lovely and
comforting as were all the staff in radiology. My girlfriend of one year was on
her way to pick me up anyway as it was my last day in that location and we had
the weekend planned together.
I also called up my mum between the CT and the MRI. she was a
radiotherapist for her whole career and so I explained the situation and asked her
to travel the 3.5 hour journey because I’d probably need my parents that night.
Her immediate realisation of the seriousness without needing to explain a
single thing was extremely helpful as i'm sure explaining the situation to your
families is the hardest part of the whole process, and mine was made so
extremely easy. Mum can do it!
sitting still in the mri scanner for half an hour whilst mid panic attack was quite an experience. The head unit in the scanner had a mirror attached to help patients with claustrophobia, this meant I could see into the control room and watch the radiographers scan me and talk me through the scan keeping me calm. By the time I left the scanner I was completely fine and calm and the radiographers had done just a fantastic job of keeping me from loosing my mind. The comfort of having people I knew go through it with me was something I can’t be more thankful for. I didn’t feel alone at all. I cant imagine just how dreadful going through something like this is for the rest of you when feeling so on your own.
sitting still in the mri scanner for half an hour whilst mid panic attack was quite an experience. The head unit in the scanner had a mirror attached to help patients with claustrophobia, this meant I could see into the control room and watch the radiographers scan me and talk me through the scan keeping me calm. By the time I left the scanner I was completely fine and calm and the radiographers had done just a fantastic job of keeping me from loosing my mind. The comfort of having people I knew go through it with me was something I can’t be more thankful for. I didn’t feel alone at all. I cant imagine just how dreadful going through something like this is for the rest of you when feeling so on your own.
Upon leaving the mri scanner I saw both my lovely girlfriend and
my fellow student who had been instrumental in running me around in her car
that week when I was feeling weak and quite a few of the radiology staff. Lisa, my student buddy had been busy behind the scenes booking my parents a B&B for the night. The
mixture in facial expressions was quite priceless between people trying to put
on positive faces and others who had just face dropped. But everyone was lovely
and said the right things and I was wheeled back down to A&E while a bed
was made ready for me on the stroke ward, I was in shock but I felt surprisingly
steady mentally. I had the right people around me.
"don't worry, it isn't that bad"
too the radiographer who said that on my way out, thankyou. never has a sentence comforted me more than that. I was a mess and this truly gave me a couple hours of stable peaceful thinking that I needed while I waited in A&E.
when I reached the stroke ward I called up my neighbour in halls who is a lovely Christian Malaysian doctor and he came straight over and we had a bit of a chat about what had happened and he told me what would likely happen now and what would be going on behind the scenes. The nurses on the ward were extremely friendly and smiley and I couldn’t have been more thankful to be living in the UK under the NHS. After a couple hours a familiar doctor appeared who I’d worked with several times in the past few weeks and he seemed very taken aback to be seeing me as his patient. But he’d come up to give me the diagnosis. He was extremely good with me and my friends who were around me at the time.
"don't worry, it isn't that bad"
too the radiographer who said that on my way out, thankyou. never has a sentence comforted me more than that. I was a mess and this truly gave me a couple hours of stable peaceful thinking that I needed while I waited in A&E.
when I reached the stroke ward I called up my neighbour in halls who is a lovely Christian Malaysian doctor and he came straight over and we had a bit of a chat about what had happened and he told me what would likely happen now and what would be going on behind the scenes. The nurses on the ward were extremely friendly and smiley and I couldn’t have been more thankful to be living in the UK under the NHS. After a couple hours a familiar doctor appeared who I’d worked with several times in the past few weeks and he seemed very taken aback to be seeing me as his patient. But he’d come up to give me the diagnosis. He was extremely good with me and my friends who were around me at the time.
He didn’t beat about the bush. Just came out and told me I
had a glioma. He treated me like I had a medical background and treated me with
a lot of respect and empathy. It was a painful pill to swallow but I can’t
imagine a nicer way to hear it, and I knew already so it made it easier. But hearing
the words from a doctor rather than your own paranoia really pounds it home. the doc left me with his number and details and said anytime. i felt extremely well looked after.
my parents turned up not long after and had been told before they reached me. Mum saw the scans and said shes seen worse. I had refused to see the scans at this point as I was too scared to look at my own mortality like that. I would later look at the scans that night as curiosity and my job got the better of me. The tumour was a large tumour in the right frontal lobe with some mild mid line shift but not too much uptake of the contrast. The worst part of it is that it’s pushing on the corpus callosum.
my parents turned up not long after and had been told before they reached me. Mum saw the scans and said shes seen worse. I had refused to see the scans at this point as I was too scared to look at my own mortality like that. I would later look at the scans that night as curiosity and my job got the better of me. The tumour was a large tumour in the right frontal lobe with some mild mid line shift but not too much uptake of the contrast. The worst part of it is that it’s pushing on the corpus callosum.
 |
| T2 |
 |
| T2 |
I was being admitted and had a four day wait till the MDT
meeting in Cardiff decided what to do. I was put on the following drugs.
16mg dexamethasone (anti-odema)
30mg ppi lansoprazole (counter stomach acid)
250mg keppra (anti-seizure)
40mg propranolol (already on it)
Had lots of support and visitors from
family/friends/colleagues. Was a very touching, emotional weekend. Was still
deep in shock but felt fairly upbeat considering the news. My grandparents had
booked a 5 sleeper 5 star cottage in the area 9 months ago out of complete
coincidence for that week and weekend which was extremely important as the town
had a festival on that weekend and there were no B&B rooms available so my
family all had somewhere to stay at night all week. It was a very busy four
days with constant visitors and I was extremely knackered. But still in shock,
which really is a lovely emotional barricade that your body throws up. I was
making jokes and was pretty jovial really. No-one found me particularly funny
but they never do anyway.
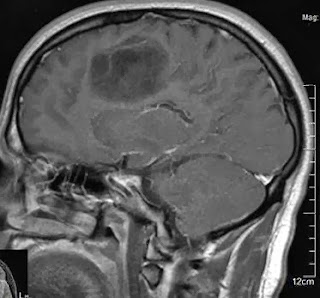 |
| post contrast scan showing low uptake |
Upside
I believe the best thing has happened to me in the
past two years is working in hospitals on a regular basis. It has given me such
a sense of perspective in terms of dealing with things like this. I’ve seen so
many hundreds of people in worse condition than me. The feelings I’m going
through aren’t why me, but really why not me. Everyone has bad luck, most
families get hit with a big smack in the face such as this eventually. I’ve had
a fairly privileged life so far. I’ve done okay. I’m finding the thought of not
having children quite desperately sad. But we don’t know whats going to happen.
Can’t think like that yet.
Subscribe to Ben's Brain Tumour Blog by Email


Comments
Post a Comment